Understanding Subgaleal Hematoma In Adults: Causes, Symptoms, And Treatment
This condition occurs when blood accumulates in the space between the skull and the scalp, often due to trauma or injury. While it is more commonly associated with newborns during childbirth, adults can also develop this condition, albeit less frequently. The accumulation of blood can lead to significant swelling, discomfort, and, in severe cases, complications that may affect brain function. Understanding the symptoms, causes, and treatment options for subgaleal hematoma is crucial for early diagnosis and effective management. A subgaleal hematoma in adults can arise from various factors, including blunt force trauma, falls, or even certain medical procedures like lumbar punctures or scalp surgeries. The condition may initially present with mild symptoms, such as localized swelling or a feeling of tightness on the scalp, but can escalate quickly if left untreated. Recognizing these signs early can help prevent complications such as infection, excessive blood loss, or even neurological issues. Since the condition is relatively uncommon in adults, many people may not be aware of its potential severity, making education and awareness essential. In this article, we will explore the intricacies of subgaleal hematoma in adults, covering everything from its causes and symptoms to diagnostic methods and treatment options. We’ll also address frequently asked questions to provide a comprehensive understanding of this condition. Whether you’re a healthcare professional, a patient, or simply someone interested in medical knowledge, this guide will equip you with the information you need to navigate this condition confidently.
- What is a Subgaleal Hematoma in Adults?
- What Causes Subgaleal Hematoma in Adults?
- How is Subgaleal Hematoma Diagnosed?
- Symptoms and Signs to Watch For
- What Are the Treatment Options for Subgaleal Hematoma?
- Can Subgaleal Hematoma Be Prevented?
- Potential Complications and Risks
- Frequently Asked Questions About Subgaleal Hematoma
What is a Subgaleal Hematoma in Adults?
A subgaleal hematoma in adults refers to the accumulation of blood in the potential space between the skull and the scalp, known as the subgaleal space. This condition is relatively rare in adults compared to infants, where it is more commonly observed due to the trauma of childbirth. In adults, the condition typically arises as a result of significant head trauma, surgical procedures, or coagulation disorders. The subgaleal space is a loose connective tissue layer that allows the scalp to move freely over the skull, but when blood accumulates here, it can cause swelling, pain, and other complications. The mechanism of a subgaleal hematoma involves the rupture of blood vessels, primarily the emissary veins, which connect the intracranial venous sinuses to the veins in the scalp. When these vessels are damaged, blood leaks into the subgaleal space, leading to the formation of a hematoma. Unlike other types of hematomas, such as epidural or subdural hematomas, a subgaleal hematoma is confined to the scalp and does not directly involve the brain. However, the pressure caused by the expanding hematoma can still pose risks, especially if it compresses nearby structures or leads to significant blood loss. Understanding the anatomy and pathophysiology of subgaleal hematoma is essential for proper diagnosis and treatment. While the condition itself is not life-threatening in most cases, its potential complications—such as infection, anemia, or even neurological deficits—make it a condition that warrants careful attention. Early recognition of symptoms and timely medical intervention are key to preventing adverse outcomes.
Key Characteristics of Subgaleal Hematoma
A subgaleal hematoma in adults is characterized by several distinct features that differentiate it from other types of head injuries or hematomas. Here are the key characteristics:
Read also:Jacob Lofland Net Worth Unveiling The Actors Career And Financial Journey
- Location: The hematoma is confined to the subgaleal space, which lies between the periosteum of the skull and the galea aponeurotica (a tough layer of connective tissue in the scalp).
- Appearance: The swelling caused by the hematoma is often diffuse and can extend across a large area of the scalp, making it visually distinct from localized hematomas.
- Symptoms: Patients may experience scalp tenderness, a sensation of fullness, or visible swelling. In severe cases, symptoms like dizziness, headaches, or even signs of anemia may occur due to significant blood loss.
- Risk Factors: Individuals with bleeding disorders, those on anticoagulant medications, or those who have sustained head trauma are at a higher risk of developing this condition.
Why Is It Important to Understand Subgaleal Hematoma?
Understanding the nature of subgaleal hematoma in adults is crucial for both healthcare providers and patients. Misdiagnosis or delayed treatment can lead to complications such as infection, chronic pain, or even systemic issues like anemia. Moreover, the condition can mimic other medical issues, such as scalp infections or superficial hematomas, making accurate diagnosis essential. By familiarizing yourself with its characteristics, you can ensure timely intervention and better outcomes.
What Causes Subgaleal Hematoma in Adults?
The causes of subgaleal hematoma in adults are diverse and often linked to trauma or underlying medical conditions. While the condition is rare, certain risk factors and triggers can increase the likelihood of its occurrence. Understanding these causes is critical for both prevention and early diagnosis. Below, we explore the primary factors that contribute to the development of subgaleal hematoma in adults.
1. Trauma to the Head
Blunt force trauma is one of the most common causes of subgaleal hematoma in adults. This can occur due to falls, car accidents, sports injuries, or physical altercations. When the scalp is subjected to significant force, the emissary veins connecting the intracranial venous sinuses to the scalp veins can rupture, leading to blood accumulation in the subgaleal space. The severity of the trauma often correlates with the size and extent of the hematoma.
Examples of Traumatic Events
- Falls from heights or slipping on slippery surfaces.
- Motor vehicle accidents, especially those involving head injuries.
- Contact sports like football or boxing, where head injuries are common.
2. Medical Procedures
Certain medical procedures involving the scalp or skull can inadvertently lead to the development of a subgaleal hematoma. For instance, surgeries such as craniotomies, scalp biopsies, or even lumbar punctures can damage blood vessels in the subgaleal space. Additionally, the use of anticoagulant medications during or after these procedures can exacerbate the risk of bleeding.
Procedures That May Increase Risk
- Neurosurgical operations involving the skull.
- Scalp surgeries or invasive diagnostic procedures.
- Use of anticoagulants or blood-thinning medications.
3. Coagulation Disorders
Individuals with coagulation disorders, such as hemophilia or von Willebrand disease, are at a heightened risk of developing subgaleal hematomas. These conditions impair the body’s ability to form blood clots, making even minor injuries or procedures more likely to result in significant bleeding. Similarly, patients on anticoagulant therapy, such as warfarin or heparin, may also experience spontaneous bleeding into the subgaleal space.
How is Subgaleal Hematoma Diagnosed?
Diagnosing a subgaleal hematoma in adults requires a combination of clinical evaluation and diagnostic imaging. Given the rarity of the condition, it is often misdiagnosed as a superficial scalp hematoma or another type of head injury. However, with the right approach, healthcare providers can accurately identify the condition and rule out other potential causes of scalp swelling or pain.
Read also:What Are Examples A Comprehensive Guide To Understanding And Using Examples Effectively
Clinical Assessment
The first step in diagnosing a subgaleal hematoma is a thorough clinical assessment. Physicians will examine the scalp for signs of swelling, bruising, or tenderness. They may also inquire about recent head trauma, medical procedures, or underlying health conditions that could predispose the patient to this condition. A detailed medical history is crucial for identifying potential risk factors.
Key Questions During Clinical Assessment
- Have you experienced any recent head injuries or trauma?
- Are you currently taking any blood-thinning medications?
- Do you have a history of bleeding disorders or coagulation issues?
Imaging Studies
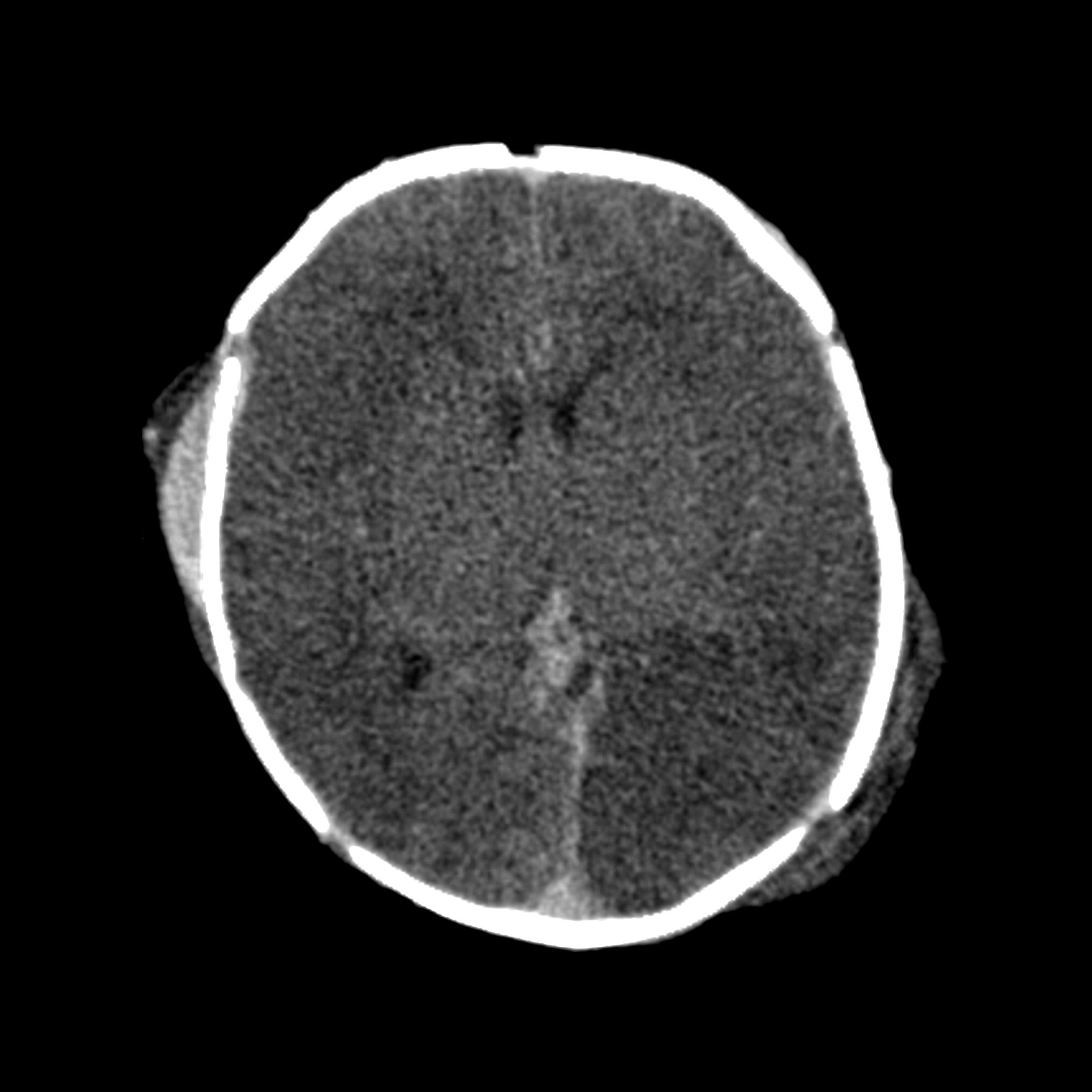
Imaging studies play a vital role in confirming the diagnosis of a subgaleal hematoma. Computed tomography (CT) scans and magnetic resonance imaging (MRI) are the most commonly used tools for visualizing the extent of the hematoma. These imaging techniques allow healthcare providers to differentiate between a subgaleal hematoma and other types of hematomas, such as epidural or subdural hematomas, which may require different treatment approaches.
Why Imaging is Essential
Imaging not only confirms the presence of a hematoma but also helps assess its size, location, and potential impact on surrounding structures. This information is critical for determining the appropriate treatment plan and monitoring the patient’s progress over time.
Symptoms and Signs to Watch For
Recognizing the symptoms of a subgaleal hematoma in adults is essential for early intervention. While the condition may initially present with mild symptoms, it can progress rapidly if left untreated. Below, we outline the most common signs and symptoms associated with this condition.
1. Scalp Swelling
One of the hallmark symptoms of a subgaleal hematoma is swelling on the scalp. This swelling is often diffuse and can extend over a large area, making it distinct from localized hematomas. The scalp may feel soft or spongy to the touch, and the swelling may worsen over time as more blood accumulates in the subgaleal space.
2. Pain and Tenderness
Patients with a subgaleal hematoma often report pain or tenderness in the affected area. This discomfort can range from mild to severe, depending on the size of the hematoma and the extent of the underlying trauma. In some cases, the pain may radiate to other parts of the head or neck.
3. Signs of Anemia
In severe cases, a subgaleal hematoma can lead to significant blood loss, resulting in symptoms of anemia. These may include fatigue, dizziness, shortness of breath, and pale skin. Recognizing these signs early is crucial for preventing complications and ensuring timely treatment.
What Are the Treatment Options for Subgaleal Hematoma?
Treating a subgaleal hematoma in adults depends on the severity of the condition and the presence of any underlying complications. In most cases, conservative management is sufficient, but more severe cases may require surgical intervention. Below, we explore the various treatment options available.
1. Observation and Monitoring
For small hematomas with minimal symptoms, observation and monitoring may be the primary course of action. Healthcare providers will closely monitor the patient for any changes in symptoms or complications. Regular follow-up appointments and imaging studies may be recommended to ensure the hematoma resolves on its own.
2. Medication
In cases where bleeding is a concern, medications such as tranexamic acid may be prescribed to help control bleeding and promote clot formation. Additionally, pain relievers may be recommended to manage discomfort and improve the patient’s quality of life during recovery.
3. Surgical Intervention
For larger hematomas or those causing significant complications, surgical intervention may be necessary. This can involve draining the accumulated blood to relieve pressure and prevent further complications. In some cases, surgical exploration may be required to identify and repair the source of bleeding.
Can Subgaleal Hematoma Be Prevented?
Preventing
Exploring The Vibrant Temple Bar Ireland Live Cam Experience
What Is Tofu Made From? A Comprehensive Guide To Understanding This Versatile Ingredient
Unlocking Knowledge: A Comprehensive Guide To The Learning Exchange VUMC

Subgaleal Hematoma In Adults
subgaleal hematoma pacs